Myths about Schizophrenia
Myths about Schizophrenia
Although schizophrenia was first described over a hundred years ago and we have been studying it closely ever since, we still do not fully understand it. Consequently schizophrenia is surrounded by more than its fair share of myths about its causes and features. Here are a few of them:
1. People with schizophrenia are always dangerous
It is one of the commonest and most enduring myths around schizophrenia that all people suffering from this condition become dangerous. Whilst the myth is not founded, it is the case that people living with schizophrenia are more at risk of dangerous behaviour such as suicide or violence when they are poorly.
Studies have found that between 10 and 23% of people who are experiencing acute psychosis may exhibit violent behaviour and this probably accounts for around 30 homicides out of a total of about 600 per year in the UK.1,2 Whether this is proportionately more than the general population, taking into account the young age group of people with schizophrenia, remains a matter of some debate.
Schizophrenia is predominantly an illness of young people: 70% of all cases being diagnosed between the ages of 16 and 25. It also happens that most violent crime is carried out by young people. So although the proportion of homicides committed by people with schizophrenia is greater than the incidence of schizophrenia in the population as a whole, the statistics are skewed by the age of the attacker and it is by no means clear that people with schizophrenia are more likely to commit violent crimes than people who do not have the condition.

Suicide by people with schizophrenia accounts for as many deaths in the UK as traffic collisions. (Image: Shutterstock)
Thankfully homicide remains a comparatively small part of the overall mortality rate for this condition. The much larger part is the problem of suicide in schizophrenia which accounts for between 800 and 1,800 deaths annually (on a par with road accidents)15. This tragically high figure represents about one in 10 of those diagnosed.
With these figures in mind it is safe to conclude that most people with schizophrenia will never exhibit dangerous behaviour of any kind and that when they do they are much more likely to harm themselves than to harm other people.
More about this subject is available in our information sheet on dangerousness.
2. Schizophrenia is very rare
Schizophrenia affects people from all walks of life and social backgrounds. It exists in all races and societies and strikes people in all age groups. The average incidence is about one percent. That is to say that about one person in every 100 will experience an episode of the illness at some time during their life.13 Today, about 280,000 people are being treated for the condition by the NHS in the UK. So the condition is much more common than many people think.
3. Schizophrenia is caused by a bad upbringing
In particular bad mothering was thought to cause schizophrenia in offspring for much of the 20th century. This belief found widespread support from the followers of Sigmund Freud’s psychoanalytic theories but it is worth noting that Freud himself believed that schizophrenia probably had physical origins and refused to treat it by psychoanalysis.
The various psychoanalytic theories reflected the belief that traumatic experiences in early childhood, often forgotten and unacknowledged, affected the development of the child’s “ego”. Later, so the theory goes, under the stress of adolescence the ego disintegrates and the person regresses to an infantile condition.3

Freida Fromm-Reichman the German psychoanalyst who saw the family upbringing as being the cause of schizophrenia.
In 1948 Fromm and Reichman took this a stage further and came up with the concept of schizophrenogenic families. That is a family environment that gives rise to schizophrenia in the offspring. In the 1960s and 1970s the growth of the anti-psychiatry movement gave the belief added impetus.
In the past such family theories have been widespread amongst professionals who have seen the person’s family as being part of the problem rather than as an important factor in the overall therapeutic solution. Families were often denied information about their loved one’s condition and people suffering from psychotic episodes were sometimes removed from their supportive family home to live in seedy bedsits where they were often unable to cope with the pressures of everyday life and were targetted by predatory or anti social neighbours. The families were then stigmatised as being the cause of their loved ones problems. The theories which gave rise to these abuses were often not tested by evidence and thankfully we have left them behind. However it is still possible to occasionally encounter older professionals who stubbornly cling to these beliefs.
3. Schizophrenia is caused by abuse during childhood
With society’s growing awareness of the issue of child abuse during the 1990’s and into the 21st century came the hypothesis that experiences of abuse during childhood and adolescence caused schizophrenia later in life. Whilst such experiences of abuse are undoubtedly psychologically damaging there is currently no research evidence of a link with schizophrenia.
In fact the theory that trauma in earlier life can cause schizophrenia later is not new and has been around since the nineteenth century. It has been the subject of a good deal of research particularly during the latter half of the twentieth century. The weight of evidence suggests that the link does not exist.4 This is perfectly logical, after all if childhood trauma did cause schizophrenia later in life we would expect to see epidemics of schizophrenia amongst groups like concentration camp survivors or the victims of the blitz and that simply did not happen.
4. Schizophrenia is just a sane reaction to an insane world
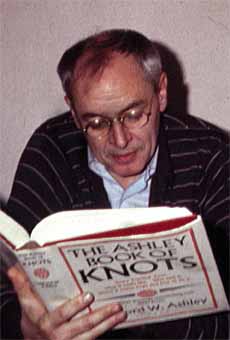
British psychoanalyst R.D. Laing who became the doyen of the anti-psychiatry movement of the 1960’s. (Image: Robert E. Haraldsen)
This bizarre theory was the brainchild of British psychoanalyst Ronald Laing who became the doyen of the anti-psychiatry movement of the 1960’s. The theory grew out of the idea that often the person diagnosed with schizophrenia was the scapegoat for the social turbulence of a dysfunctional family environment and may in fact paradoxically be the sanest member of the family group. Although this idea gained a great deal of popularity, in later life Laing himself became increasingly disillusioned with it.5
5. Schizophrenia doesn’t exist

Dr Thomas Ssasz, American psychoanalyst who believed that schizophrenia was a myth. (Image: Jennyphotos)
In the middle of the 20th century there were those in the anti-psychiatry movement who proposed that schizophrenia didn’t exist at all and that it was simply an invention of the psychiatry profession. Dr Thomas Szasz a psychoanalyst in the USA became well known for this theory. He called schizophrenia a fake disease and the sacred symbol of psychiatry.6 Perhaps if he had ever had to endure a day living with the voices he would not have resorted to this strange notion.
6. Anti-psychotic medication is just a chemical cosh
Although the early anti-psychotics (called typical) did have sedating effects and in high doses could cause people on them to become slow and lethargic, anti-psychotics are not used principally for that effect but for the benefit that they bring in helping to alleviate the positive symptoms of schizophrenia such as the delusions and hallucinations.8

Chlorpromazine (Largactil) the first of the antipsychotic drugs.
Unfortunately these early antipsychotics were often misleadingly called “major tranquillisers”, a term which has stuck to this day and unfortunately leads to much confusion about their role. When the first psychiatrists to study their use, the Frenchmen Jean Delay and Paul Deniker, first used the antipsychotic chlorpromazine in psychiatry, it was precisely the fact that the drug had a more precise effect in calming their patients than the other tranquillisers in use at the time, that attracted them to it. It was later found that this effect was not due to sedation but because the chlorpromazine acted directly to reduce the hallucinations and delusions. 14

Before the advent of the antipsychotic drugs most people with a diagnosis of schizophrenia were confined in one of the large asylums, like this one on the edge of Dartmoor, sometimes for many years. (Image: Guy Wareham)
The beneficial humanitarian affect of the antipsychotic drugs should not be underestimated. Before the introduction of these drugs in the UK about 70% of people with a diagnosis of schizophrenia were continuously confined in mental hospitals: today it is only about 5%. 14
The more modern atypical forms of anti-psychotics have less sedating effect and are preferred nowadays over the older type of typical ones. The guidance given by NICE to NHS doctors working in the UK is that newer atypicals should be used in preference to the older typicals in new cases of schizophrenia, where the person is acutely ill or where side effects are being experienced from the use of an older typical drug. 7
7. Schizophrenia is a split personality
One of the popular myths about schizophrenia is that it involves a split personality: a Jekyl and Hyde personality. This is not the case. Although the term schizophrenia literally means a split mind and was coined by Dr Eugen Bleuler, a Swiss psychiatrist, the condition does not really manifest itself in that way. It would be more accurate to regard the condition as one in which the mind becomes confused and disordered. 8
8. People with schizophrenia will be severely disabled for life
Whilst in theory this shouldn’t be so, in practice there is, at least in the UK , some truth in this.
Our experience of schizophrenia from over a century of study tells us reliably that about 25% of people who experience an episode of psychosis will go on to recover completely and have no further problems in their life. We also know now that given proper treatment a large proportion of the remainder will be substantially recovered and will go on to achieve a high level of functioning. 9
Yet in the UK today only about 13% of people with a diagnosis of schizophrenia are in any kind of work.10 So clearly there is an enormous disparity between the clinical outcomes and the social outcomes. Why is this so? Clearly this is an area that needs much greater study, in particular in view of the fact that the number of people with schizophrenia in work at the moment in the UK is actually declining.
There may be a number of factors at work here. Some would blame a benefits culture that gives people “on the sick” very few incentives to seek work. Others would blame the stigma that people with schizophrenia face from employers when looking for work.
Another factor may be arguably that many of those professionals caring for people with schizophrenia see permanent unemployment as being the natural lifestyle for people with a diagnosis of schizophrenia and have little ambition for the people in their care. Others may be loathe to put their patients under the stress of looking for work in an increasingly competitive jobs market for fear of provoking a relapse in their condition.
Whatever the reason we believe that this issue is an area that should become absolutely key in our study of this condition and development of our treatment models in future years. Many thousands of bright and intelligent people who could be making a creative contribution to the wellbeing and prosperity of our society are currently consigned to a life of low achievement because of these issues. After all other countries, notably Italy and Cuba, have much better outcomes in terms of employment for people living with schizophrenia.
This is not however a problem unique to people with schizophrenia. Most people with physical disabilities also experience other people in society who wrongly assume that they are incapable of achieving.
9. If it’s genetic, then we can do nothing about it
Research has shown that there are a number of factors that can contribute to a successful recovery including reducing family stress, useful occupation, talking therapy and reducing stress from financial problems.11
We also know that early diagnosis and treatment with antipsychotic medication will improve prospects of a good recovery enormously. 12 Another factor that is crucial to a successful recovery is having a good recovery strategy. Living one day at a time may be an appropriate strategy for coping with a crisis but later it is necessary to start identifying goals in your life and plotting a path towards achieving those goals.8
Having a genetic predisposition to suffering with schizophrenia in no way guarantees that you will suffer from it and even if you do there is no need for an episode of schizophrenia to necessarily be a life sentence.
10. If it’s genetic, then let’s get rid of the bad genes

Hartheim Euthanasia Centre in Germany where over 18,000 people with disabilities including people with schizophrenia were killed during the Third Reich. (Image: Dralon)
This was of course exactly what the Germans tried to achieve during the Third Reich. Then people with schizophrenia were simply killed by the use of gas chambers in the hope that the defective genes could be eliminated from the race.
Apart from the humanitarian and ethical considerations, this approach has three serious flaws. First of all it is not clear whether the genetic factor consists of one gene acting alone or several acting in combination so the process is almost certainly more complicated than may appear at first sight.
Secondly, as we have said before, simply having the right genes for schizophrenia in no way guarantees that you will suffer from it yourself. For instance, if you are an identical twin with a sibling who has schizophrenia you only have a 50% chance of suffering from it yourself even though you share all the same genes.
And lastly, genes with adverse affects on the species tend to be bred out of the gene pool during the natural process of evolution and the fact that the schizophrenia gene has survived this long implies that it must impart beneficial traits to the species in addition to the adverse one. Eliminating the schizophrenia gene would therefore almost certainly cause as much harm to the gene pool as benefit. There is already some prima facie evidence for this. People with schizophrenia are thought to have a reduced incidence of certain physical illnesses such as rheumatoid arthritis and some cancers.
It is also worth remembering that during most of the twentieth century, the practice both in the UK and USA was to confine people with schizophrenia in one of the large mental asylums where they had very little opportunity to reproduce. Yet during that time the incidence of schizophrenia in those countries actually increased slightly. So clearly the genetic issue is more complicated than we may at first infer.
Conclusion
Sadly schizophrenia attracts many ideas and beliefs that just don’t stand up to the evidence. Over the last hundred years we have accumulated an enormous amount of research evidence to guide the way that we treat and respond to schizophrenia. However it still receives less research funding than other physical conditions such as heart disease or cancer. If we are to finally blow away all of these myths and the others that will surely follow in their path we need governments to fund much more research into this life changing condition.
References
1. Fazel S, Reinharth J, Serper M, Singh J, 2011, Structured Assessment of Violence Risk in Schizophrenia and Other Psychiatric Disorders: A Systematic Review of the Validity, Reliability, and Item Content of 10 Available Instruments, Published in Schizophrenia Bulletin September 2011.
2. Rollin H, 1980, Schizophrenia at Home, Published in Coping with Schizophrenia, Burnett Books. P23.
3. Howe G, 1986, Schizophrenia A Fresh Approach, David & Charles, P26.
4. Fuller Torrey E, 2001, Surviving Schizophrenia, Quill, P166.
5. Fuller Torrey E, 2001, Surviving Schizophrenia, Quill, P171.
6. Fuller Torrey E, 2001, Surviving Schizophrenia, Quill, P171.
7. Reveley A, 2006, Your Guide to Schizophrenia, Hodder Arnold, P74.
8. Author’s personal experiences.
9. Fuller Torrey E, 2001, Surviving Schizophrenia, Quill, P130.
10. Warner R, 2000, The Environment of Schizophrenia, Brunner Routledge, P73.
11. Jones S and Hayward P, 2004, Coping with Schizophrenia, One World, P45.
12. Howe G, 1991, The Reality of Schizophrenia, Faber and Faber, P61.
13. Reveley A, 2006, Your Guide to Schizophrenia, Hodder Arnold, P13.
14. Cutting J and Charlish A, 1995, Schizophrenia, Thorsons, P124.
15. Accurate figures of deaths by suicide amongst people with schizophrenia are difficult to derive. However by drawing on various UK and US sources a suicide rate in schizophrenia of 300 to 600 per 100,000 per year seems to be a good and close approximation.