Religious and Spiritual Delusions in Schizophrenia
For many people religion is one way that we understand the world and give meaning to our lives and certainly religion and spirituality play an important part in many people’s experiences of schizophrenia. For some sufferers religious delusions or intense religiously-based irrational thinking may be a component of their symptoms, for instance they may believe that they have been sent by God to become a great prophet. However for other people religion and spirituality play an important role in their recovery process. They may find that their spiritual beliefs and practices help them to make sense of the world in a way that they could not when they were suffering from psychotic delusions and that membership of a supportive faith community provides vital fellowship when faced by the everyday problems of living with a serious mental health condition.
In this series of information sheets we look at spirituality from a number of different perspectives both when it becomes a problem as in religious delusions and when it becomes a supportive component of a recovery process.
What are religious Delusions?
In this page we look at how religious delusions manifest themselves in many people suffering from the effects of psychotic thinking. In our related information sheets such as Spirituality in Schizophrenia: A Christian Perspective, other writers give their own accounts of how their spiritual and religious beliefs have helped them.

It is often said that a person with schizophrenia will go to see a priest before they see a psychiatrist. (Image: Kzenon on Shutterstock)
It is often said that a person experiencing the first stages of serious schizophrenia is more likely to go to see a priest than a psychiatrist1. This is because the delusions suffered by people with schizophrenia often have a religious content. Sufferers may believe that they are a saint, a prophet or God himself, (which is more common in men), or (in women) that they are a saint or are pregnant with the Messiah.
Sometimes the person may believe that they are being punished for some unforgivable sin that they have committed earlier in their life or that they are damned to everlasting hell.2 This can lead to feelings of intense despondency. In other cases the sufferer may believe that others around them are devils or witches and may attack them or that they themselves are possessed by devils.
There is an amusing story from the 1980s of two patients meeting for the first time on a psychiatric ward who, after telling each other their story immediately fell into an altercation with one patient accusing the other of being an imposter: “how can you be Jesus Christ?” he said, I am Christ.2.
How common are religious delusions in schizophrenia?
Various studies have found that the prevalence of religious delusions in schizophrenia is very high. Torrey in the US, for instance, has suggested that around half of sufferers there experience religious delusions.1 Other studies in other parts of the world have found differently. Mohr and Huguelet in Switzerland found the prevalence to be around 21% (this was probably representative of the overall prevalence in Western Europe)4 and Rudaleviciene and his colleagues in Lithuania found it to be as high as 64% there.5
Whatever the figures may be for an individual country it is clearly a trait that is very common in schizophrenia and psychiatrists encounter it so frequently that they have come up with a name for it: religiosity or religious preoccupation. Religiosity is definitely not new. The early psychiatrists in the 19th century observed the phenomenon although it was not thought to be quite as common then as now.6
Religiosity and psychiatry: How is religiosity diagnosed?
Psychiatry and religion have traditionally been ill at ease with each other and in today’s increasingly secular society which the UK has undoubtedly become many mental health professionals feel uncomfortable when dealing with the issue of religiosity and have difficulty in understanding it in the context of the whole person.
These factors have made it difficult for doctors to properly diagnose religiosity. There is an example of a ward nurse in a Westcountry hospital listing a woman’s crucifix on her list of belongings as a “lucky charm”. This may be a good example of how incomplete an understanding medical professionals often have today on religious issues or it may be an example of an individual member of staff allowing her own personal secular agenda to overcome the necessity for professionalism in the practice of her vocation. Whichever, it is I believe a good example of the difficulty that many health professionals have in the UK of understanding religious practice and without such an understanding, diagnosing religiosity properly becomes very difficult.
Coverage, or to be more precise lack of it, in the medical literature has not really helped this problem. Despite religiosity being such a common experience for people with schizophrenia it is not particularly well covered by the medical literature. A review of four major psychiatric journals carried out in the US in 1982 found that only 2.5% of the articles even mentioned religiosity and that in most cases the mention was just cursory.4
Jehovah’s Witnesses believe in the imminent end of the world. It is vital; to understand a person’s cultural background when diagnosing religiosity. (Image: Shutterstock)
Religious delusions may be difficult to distinguish and diagnosis often depends on a complete knowledge of the person’s previous religious history. For instance if the sufferer has never had a religious background but has suddenly started visiting churches three times a day this would be significant whereas if previously they had attended church regularly then weekly church going would not be out of place and bear in mind that in some faiths religious observance can be quite significant and involve praying several times a day or abstaining from food at certain times.
This is a good example of how the cultural context of religiosity is vital to understanding it. In days of old and many societies in the developing world today, mental health and spirituality are seen to be closely related. Indeed the Greek word “psyche” from which we derive our terms psychologist and psychotherapy originally meant the soul or spirit.7
Excessive religious observance is often the first sign that relatives see that something is amiss. Visiting churches too frequently, praying continuously and fasting (sufferers may often loose excessive amounts of weight) when there has been no previous interest in religious activities are often a sign that something is seriously wrong.3 It is vital that doctors listen to relatives and take into account any recent changes in the person’s behaviour or lifestyle.

In diagnosing religiosity a great deal of information will be gained from the diagnostic interview between the patient and doctor. (Image: g-stockstudio on Shutterstock)
However the major part of the evidence of religious delusions will come from the diagnostic interview with the patient and any further contact that the doctor has with them. As we have seen above holding extreme religious views does not of itself indicate mental illness however doctors should look for any signs of anomalous religious behaviours or beliefs that appear to have started without any prompting and may occur in conjunction with other symptoms such as paranoia or hallucinations. Today’s guidance to psychiatrists in both the UK and US is sound and very explicit in that they must familiarise themselves with the patient’s cultural background before interpreting religious practice as delusional.
Why do people with schizophrenia experience religious delusions?

Schizophrenia is predominantly a condition of the young: a time when religious belief is in a state of flux. (Image: Halfpoint on Shutterstock)
First of all it is important to remember that schizophrenia is predominantly (but not exclusively) a condition of young people, with three quarters of all diagnoses being made between ages 16 and 25. This is a time when spiritual and philosophical beliefs are usually in a great state of flux and when the person is extremely vulnerable to deluded thinking on this issue.
It is also important to realise that all of the person’s previous ideas, beliefs and experiences form the framework for their psychotic thinking and because religion still plays an important part in our society it is not surprising that there will be a religious component within psychotic beliefs.3
But psychotic thinking is not restricted to religion; it reflects all aspects of a person’s experiences. For instance the belief widely held by many people with schizophrenia that they are being spied on by MI5 would not have existed in the 19th Century before MI5 was created. Although acknowledging that people’s previous experiences can form the framework for psychotic thinking, it is not the same as saying that it causes it. Schizophrenia is no more the result of a religious upbringing than it is the result of watching too many spy movies.
We also see cultural background reflected in the nature of the religious delusions themselves. For instance in predominantly Catholic countries the delusions will reflect Catholic belief whereas in predominately Hindu countries they will reflect Hindu ones. There are also some interesting twists on this though. For instance in Poland religious delusions in people with schizophrenia appeared to increase during the decades of Communism when organised religion came under pressure from the state. 8
Why is religiosity significant?
Some studies have found that sufferers who experience religious delusions tend to experience a more severe course of their illness with a poorer prognosis.8 In addition religious delusions and hallucinations can give rise to disturbed behaviour that can sometimes be dangerous to both the sufferer and to those around them.
Religious delusions may also be accompanied by hallucinations of a religious nature. The most common here is the phenomenon of hearing voices which the sufferer may interpret as messages from God or saints. The person may also experience visual hallucinations which they interpret as visions.
Religious delusions and hallucinations often link together and can be very powerful in the way they influence the person’s behaviour. After all if you believe that the voices that you are hearing in your head and which are giving you commands are coming from God or some other higher power then there is a powerful reason to listen to them and obey them. When we talk of hearing voices here we are not describing the normal self talk that every individual experiences. The voices that a person with schizophrenia hears are qualitatively different to that. They are true auditory hallucinations: hearing things that the hearer cannot distinguish from reality. For more about this please see our Information Sheets on Voices.
Religious delusions may also lead to dangerous behaviour. Both homicide and violence have been committed by people with schizophrenia at the behest of their religious delusions and some have taken statements from the bible to pluck out offending eyes or cut off offending body parts literally and have done themselves great harm.4
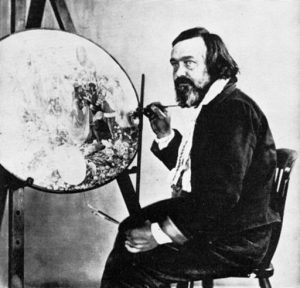
Richard Dadd the 19th Century English painter who killed his father after suffering from religious delusions. (Image: Henry Hering on Wikimedia Commons)
In 1843 at the age of 26, the noted English artist Richard Dadd killed his father believing that his father was the devil and that he (Dadd) had been called upon by God to do battle with the forces of evil. Despite being confined in asylums (first the Bethlem and then Broadmoor) for the remainder of his life, Dadd went on to do some of his best work including the famous The Fairy Fellers Master Stroke which can be seen in the Tate Gallery today.
More recent examples have included the case of a man with schizophrenia who began attending a cathedral in the Westcountry where he became infatuated with a female member of the congregation who he thought to be a saint and ended up propositioning her. 9. People suffering from religious delusions have also been encouraged to kill themselves by their delusions.
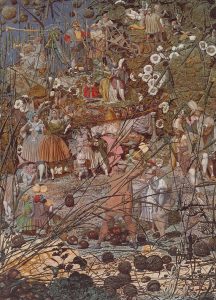
The Fairy Feller’s Master Stroke by Richard Dadd. (Image: Tate London on Wikimedia Commons)
This is not to say that all people with schizophrenia who experience religiosity will display dangerous or disturbed behaviour. That is certainly not the case. However with over 1,000 people with schizophrenia dying by their own hand in the UK each year we cannot afford to dismiss or minimise the problem of dangerous behaviour in schizophrenia and it is important that doctors and police take seriously any reports reaching them from faith communities of these kinds of problems. The key to minimising dangerous behaviour is to catch it early and make an early intervention with psychiatric treatment. Taking a wait and see approach is often disastrous.
People with Schizophrenia in Church Communities
In fact it is not uncommon for people with schizophrenia to be attracted to join church communities. Usually this presents no real problems but sometimes disturbed behaviour will become a real challenge for the congregation and church leaders alike. The person may attempt to preach or chastise members of the congregation or become otherwise disruptive. This presents the community with a real problem. How do they continue to offer help and support to someone who is clearly very ill and in need of help whilst at the same time maintaining the dignity of their place and practice of worship? Members of the clergy rarely have any training in mental health and often struggle to cope with this issue.
This Information Sheet deals specifically with the phenomenon of religious delusions in schizophrenia: a phenomenon that can cause people with schizophrenia enormous suffering. But if religious delusions are a bad thing generally for people suffering with schizophrenia what about religion in general? Is it good or bad for people living with schizophrenia? In fact there is now a considerable weight of evidence that points to religious and spiritual belief as being a broadly protective and positive factor for people living with schizophrenia and we deal with that subject in our Information Sheet.
What can be done about religious delusions?
Like most of the other delusions and hallucinations that people suffering from schizophrenia experience, the mainstay for treatment in the NHS today is medication with one of the antipsychotic medicines. These are effective in relieving the symptoms in around 70% of people who take them. There are however a number of different antipsychotics available to the doctors and finding the right drug for the particular person can often take some time and considerable patience. Talking treatments such as counselling and psychotherapy will also help and there is now an increasing recognition of their efficacy within the mental health field.
However, the relief of the symptoms is usually only a part of the recovery process. For someone who has suffered from religiosity, which was so very convincing whilst they were in the middle of their psychotic haze, the process of sorting out the delusional thinking around religion from the more rational can be a long and difficult process of self-discovery. To return to a more sane structure of religious beliefs and values following a period of intense religiously-based irrational thinking is extremely difficult. It often takes many years for the person to work this through and to finally come to an arrangement with their maker that reflects more common approaches to religious belief. At this point the clergy and church leaders can play a vital role with guidance and support.
References
1. Torrey EF, 2013, Surving Schizophrenia, Harper Perennial, P327.
2. Howe G, 1991, The Reality of Schizophrenia, Faber and Faber, p32.
3. Author’s personal experiences.
4. Mohr S and Huguelet P, 2004, The relationship between schizophrenia and religions and its implications for care, published in Swiss Medical Weekly.
5. Rudaleviciene P, Stompe T, Narbekovas A, Raskauskiene N, Bunevicius R, 2008, Are religious delusions related to religiosity in schizophrenia?, published in Medicina.
6. Frith C, Johnstone E, 2003, Schizophrenia, Oxford University Press.
7. Watkins J, Living with Schizophrenia, Hill of Content.
8. Krzystanek M, Krysta K, Klasik A, krupka-Matuszczyk I, 2012, Religious content of hallucinations in paranoid schizophrenia, published in Psychiatria Danubina.
9. This is Cornwall, www.westbriton.co.uk posted 13 January 2009.
Copyright © November 2016 LWS CIC.